UrgentCare-Cloud gives urgent care providers an all-in-one EHR and practice management platform designed for the realities of high-volume, fast-turnaround care. From intake to discharge, documentation to billing, our specialty-specific tools help you move quickly without sacrificing accuracy.
Run your urgent care center without bottlenecks. Our 4-Step Workflow ties together scheduling, charting, labs, and billing—so your team can focus on treating patients, not chasing admin tasks. Whether you’re managing acute illness, injuries, or occupational medicine visits, our templates and tools make documentation quick, compliant, and revenue-ready.
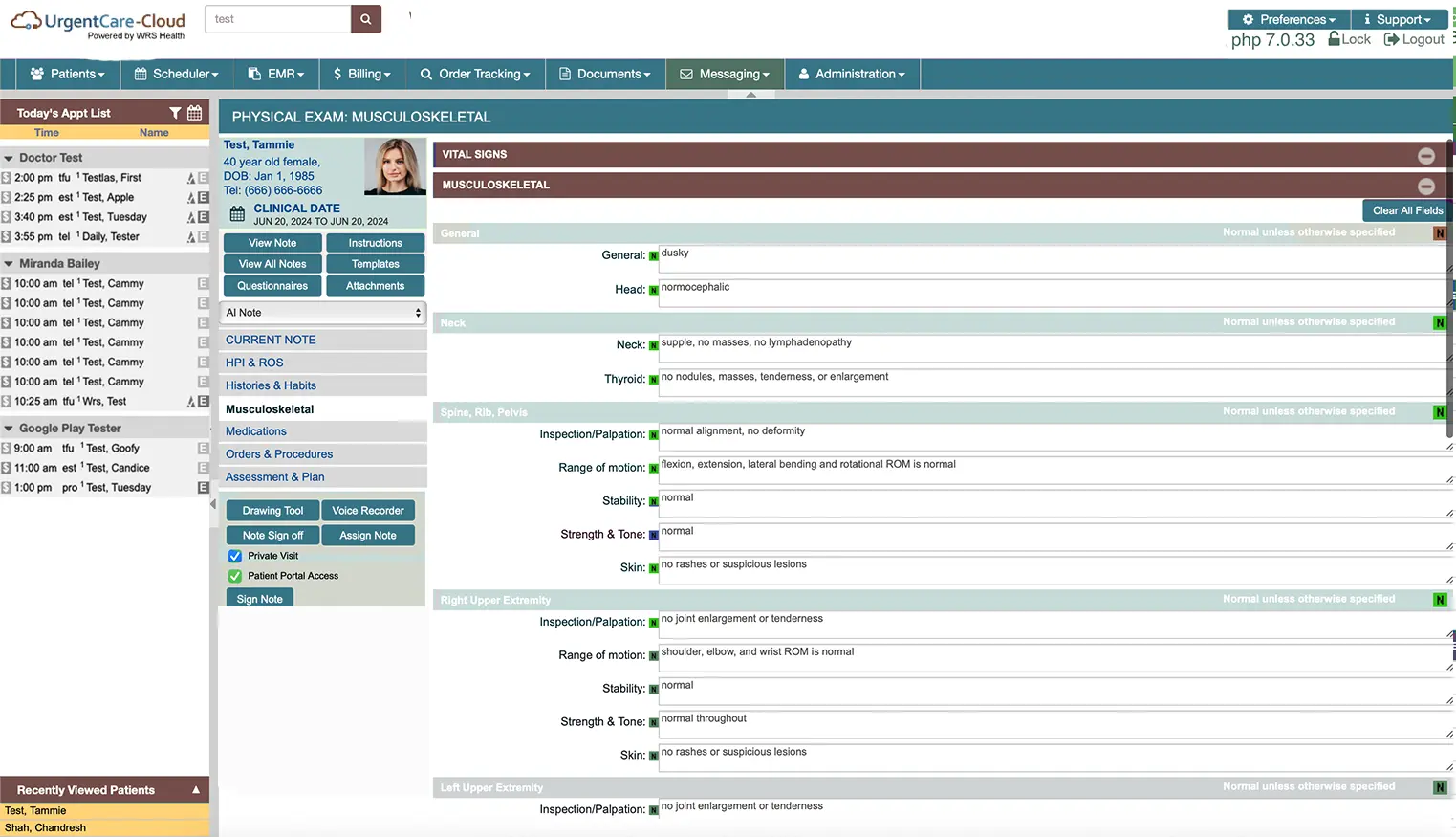
Document walk-ins and episodic care efficiently with templates for respiratory infections, lacerations, sprains, burns, and more. Pre-built order sets and visit protocols streamline everything from triage to discharge.
Support employer contracts with built-in tools for DOT physicals, drug testing, and workers’ comp claims—all seamlessly tied into patient and employer records.
Get reimbursed faster with urgent care–specific coding, real-time claim validation, and accurate charge capture for procedures like suturing, X-rays, and drug screenings.
Order and review labs or imaging directly within the EHR, with results flowing automatically into patient charts—no duplicate entry required.
Our Business Process Outsourcing (BPO) services help urgent care centers reduce admin overhead, improve revenue cycle performance, and scale without adding staff. Whether you operate a single walk-in clinic or multiple urgent care sites, we give you the tools and support to grow.

Schedule a time to talk or book a complimentary practice assessment today.